I want to explain the part of treatment I’ve been doing since November 2021 - the drugs. But cancer drugs are not sparkly and there’s not a fun story to go along with them, like there was during radiation and realizing one of your doctors is a former Goodson student. Additionally as far as the overall treatment plan, radiation was a blip on the screen, whereas the drugs make up the long game - meaning there’s a lot more to process, adjust to and come to terms with physically, mentally and emotionally given the hopefully extended duration of this part of treatment. As a side note: when I say “duration of this part of treatment,” that means as long as there’s no progression of cancer (no growth at the site in my hip and/or no new spots in rest of my body) - so fingers hard crossed for a long duration.
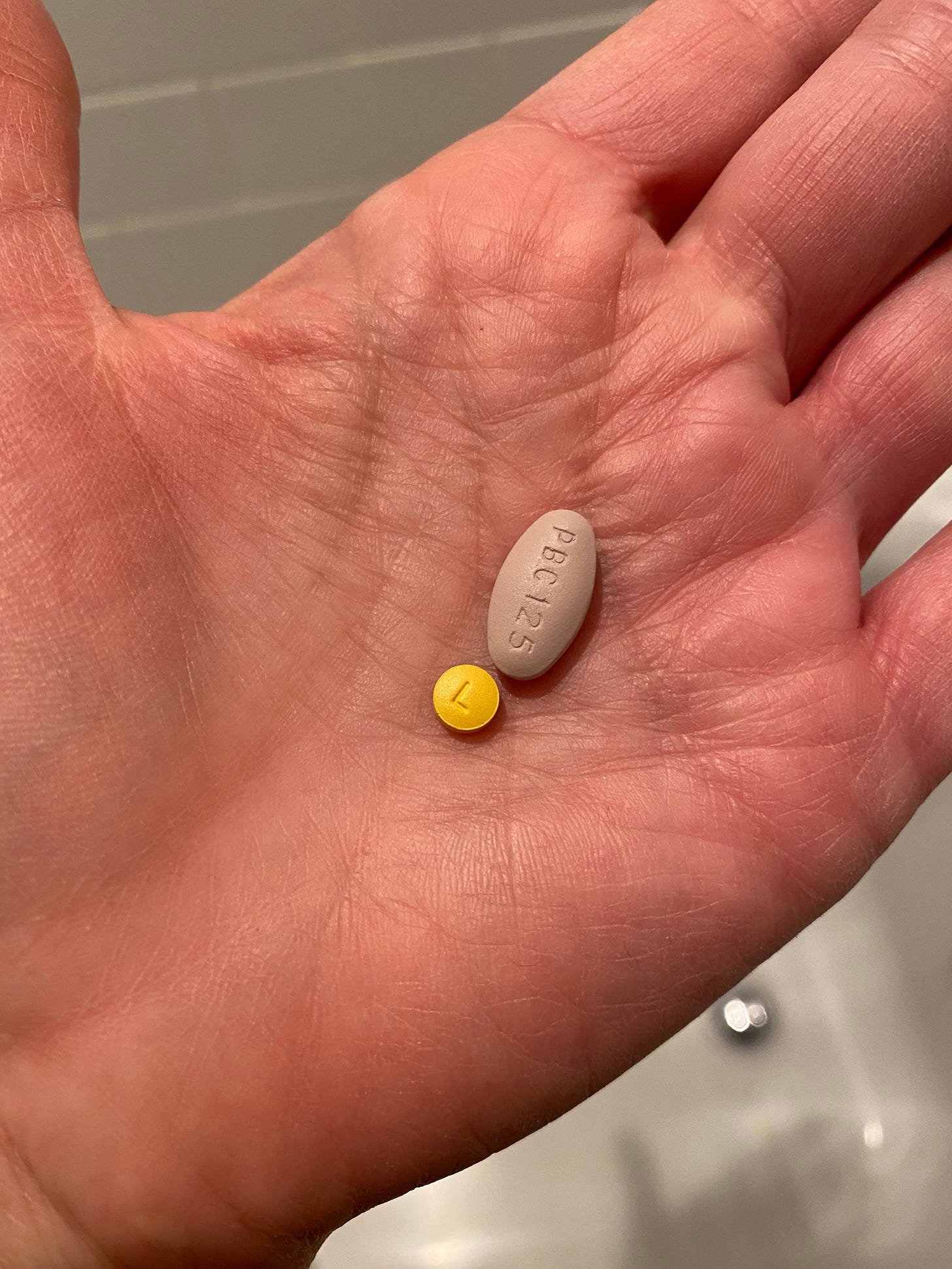
There are three drugs (Letrozole, Ibrance and Xgeva) that make up this part of my treatment. Letrozole, which I take everyday, is a hormone-suppressing drug, and because I have an estrogen-positve breast cancer that gets fuel to grow from estrogen, Letrozole decreases the estrogen available in my system. I’ve been on drugs like Letrozole in the past - Tamoxifen before menopause, Arimidex after. And because it complements Ibrance, described next, it’s why I take Letrozole.
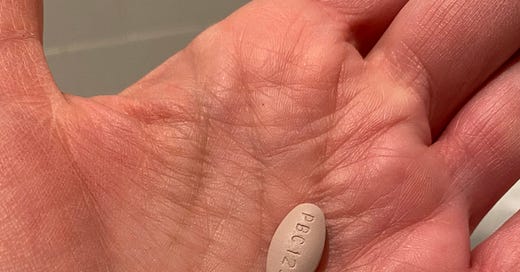
Ibrance, is what I’d call the cancer drug because it “improves progression-free survival or the amount of time after the start of treatment the cancer does not grow substantially.” Its job was described to me like this - While Ibrance won’t make the tumor disappear, like a brake pedal on a car, it keeps its foot on the tumor so cancer growth won’t accelerate. Ibrance is administered orally in 28-day cycles, a pill a day for 21 days and then seven days of no pills. It is not considered a traditional form of chemotherapy, but is referred to as a targeted treatment/therapy.
The third drug I receive is a once-per-month-or-so injection of Xgeva. The role of this drug is to slow the overactive breakdown of bone due to busy cancer cells. It helps to keep the bone intact and run less of a risk of fracture(s) to the bone.
I mentioned earlier that I’m not doing chemotherapy this time around; instead I’m doing targeted therapy. Targeted therapy and chemotherapy are not exactly the same in the way they treat cancer. Targeted therapy treats specific parts of cancer cells affecting how they grow, divide and spread, and chemotherapy hits both cancer and healthy cells. But… if you put a list of possible side effects of targeted therapy next to possible side effects of chemotherapy, both have their share of side effects that range from mild to serious. In the end, for a person who’s experienced both types of treatment, it’s, in my opinion, a tomato/tomaaato situation.
Here’s a general breakdown of how drug treatment plays out for me. While I will not lose all my hair like I did on chemotherapy, on Ibrance/Letrozole my hair has thinned. I noticed more hair from my head coming off in my hands when I washed or styled my hair for the first few months of treatment, but thanks to a good haircut and long bangs, I’m the only one who really knows that I’ve got noticeably less hair at my temples where hair loss is most obvious. I still have eyelashes and eyebrows, and I’m glad for that - I lost those during chemotherapy. My eyelashes never did grow back to their original thickness and length after chemotherapy, but I have a full set. And it seems like my eyebrows are much less dense, so thank goodness again for bangs! They do the trick here, too, by covering my thinned eyebrows! I’ve also found products for thinning hair, eyelashes and eyebrows that I put on most days, and they seem to work to encourage hair growth.
As for the rest of my body, I don’t care so much about that. Hair has thinned or disappeared altogether - not much hair remains on my arms or trunk, and what hair I have on my legs is patchy at best. But because I can’t see without cheaters and quite frankly I don’t care all that much (or wear my cheaters in the shower), I don’t bother shaving my legs anymore. During both chemotherapy and now, I thought it was a perk of the drugs to speed up shower time by not having to grab for the razor!
Thankfully, on Ibrance, my finger and toenails are intact and continue to grow as normal - they were infected and fell off during chemotherapy. Aside from month one, I haven’t had to deal with nausea - that’s a win. I don’t remember mouth sores while on chemotherapy, but on Ibrance, I’ve had them pop up almost monthly - they’re not major, and I can manage them.
The side effect that is most bothersome is chronic fatigue. In the beginning, I would find myself pretty overwrought because I was so tired - forcing and pushing myself one day (or even one part of the day) and then cratering and crashing later. Coming to terms with this is a real challenge for me, but I’m learning to redefine my days and how I do my life. I’m more willing to let myself dose off when I feel the need. Sometimes that’s a 20-minute nap; other times it’s two, three hours of dead dog, out-for-the-count, loud snoring deep sleep. I’m aware that it’s what I need, and struggling to stay awake is just not a good look on me.
One of the most concerning and closely monitored side effects of Ibrance is low WBC counts (specifically low absolute neutrophil counts). Neutropenia is common and expected when on Ibrance, and it becomes a serious issue for patients because white blood cells are what fight infection, and if WBC counts are low, then a patient is likely to have difficulty fighting an infection, and that can be quite serious.
So as a reference - the normal absolute neutrophil range is between 1.5 and 8.0. I get my monthly blood work done on Day 1 of every 28-day cycle of Ibrance. Keep in mind that Day 1 is the day when my counts are at their highest during the cycle because I’ve just finished a week of being off of Ibrance for seven days after 21 days of being on it - and during those 21 days the counts are gradually decreasing.
The results from the blood draw serve as a guide for my new doctor, Dr. Shah (see informative and important video featuring her on Good Morning America here). Also quick side bar - you might be wondering why I haven’t mentioned Dr. Cristofanilli? He moved to the east coast shortly after he and I reconnected, he found I had a recurrence and created a treatment plan for me. He’s now out east working at Cornell.
Back on track… Dr. Shah (or on alternating appointments, Nisha - her nurse practitioner) takes a look at all the numbers of various things tested, but hones in on the absolute neutrophil count (ANC). That count can drive dosing of Ibrance suggesting it might be necessary to push pause on starting a new cycle for a week so that the count can recover a bit more. And remember the normal range of the absolute neutrophil count? Well my count historically (since being on Ibrance) hovers around 0.9/1.0 - always below the normal range - so it’s no surprise about occasional mouth sores, chronic fatigue and the need to be mindful and protective so as not to get sick.
Xgeva’s side effects are kind of on the back burner - there’s no real issues for me with the drug. There is heightened concern regarding osteonecrosis (breakdown of the jaw bone), so my dental care team take good care to be sure my teeth and jaw remain in good shape. But otherwise, not a big deal with Xgeva.
In the end, are the side effects do-able? The undercurrent of tiredness? Thinning hair? Mouth sores? The blood draws? The injections? I think so. These small but mighty drugs are fighting a battle on my behalf. And knowing this means I can and will adjust to make way for them to do their job.



sending love and strength and ease--!! <3